Understanding HHT
More than a nosebleed
What you need to know before exploring more about HHT is that if you are an individual looking for additional information or a clinician wanting to learn more for a patient we always recommend that you contact your national HHT Center of expertise for the best answers and care possible. If you are unable to reach or find a Center our National Member Organizations will be happy to assist you. If you have no HHT Organization in your country please contact HHT Europe and we will offer you all the necessary assistance.
What is HHT?
Hereditary Haemorrhagic Telangiectasia is a rare genetic disorder of the blood vessels. It causes ArterioVenous Malformations (AVMs) in many vital organs.
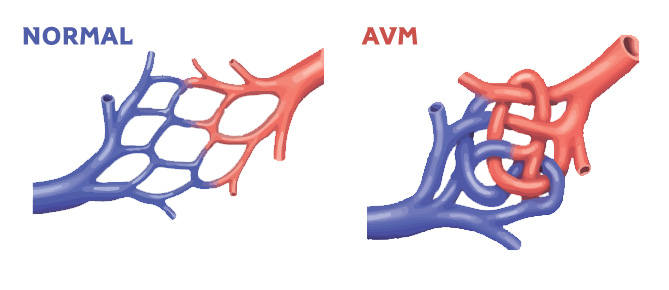
What is an
AVM?
Symptoms and obvious signs
Nosebleeds
90% of HHT patients suffer recurrent nosebleeds, which may result in anaemia and the need for
iron infusions and blood transfusions. These are small AVMs and appear like tiny red dots on the face, skin, lips, mouth and fingertips. (Other symptoms may include shortness of breath,
exercise intolerance, fatigue, migraine headaches, seizures, abdominal pain, intestinal bleeding)
Telangiectases
The manifestations of HHT are variable; patients can present with a varied combination of symptoms and signs.
The Silent Dangers
HHT
AVMs are often present in the gastrointestinal tract. They may bleed continuously, and are
difficult to locate and treat.
HHT Timeline
Screening for Pulmonary (lung) and Cerebral (brain) AVMs is essential to detect and treat when necessary and avoid a serious danger for patients during their entire life.
Newborns
Possible lung and brain AVMs at birth.
Age 12
Nosebleeds may begin. They can appear earlier, later or never at all.

Age 30 to 60
Telangiectases become more evident. Increase in nosebleeds. Possible increase in gastrointestinal bleeding.

Age 60+
Gastrointestinal bleeding may worsen. The dependence on iron infusions and blood transfusions may increase.
How is it
transmitted
It does not depend on the sex of the child or the parent.
A parent with HHT may transmit the gene; each child of an affected parent has a 50% chance of inheriting the disorder. If you don’t have HHT you cannot pass it on.
Diagnosis
A diagnosis is likely if 3 of these clinical criteria are present:
- Spontaneous & recurrent nosebleeds.
- Multiple telangiectases in typical locations (face, lips, oral cavity, fingers)
- AVMs in other organs (lungs, liver, brain, gastrointestinal tract)
- A 1st degree relative with HHT by these criteria.
Prognosis
A cure does not exist but screening for manifestations in an HHT Specialist Center can help prevent the most serious complications of HHT.
1 in 5000 people worldwide have HHT
Figures
90% of them do not have a diagnosis.
Additional Resources
- HHT International Guidelines (https://hhtguidelines.org)
- VASCERN HHT WG resources (https://vascern.eu/expertise/rare-diseases-wgs/hht-wg/)
